Early on in the COVID-19 pandemic, Penn Medicine faced two major challenges. First, they had to find a way to care for patients safely and humanely when they could not meet with them face to face. They also had to figure out how to support the broader community—including those who were not established patients—and provide accurate and up-to-date information about the virus. Team members from multiple Penn Medicine groups, including Information Services (IS), Office of the Chief Medical Information Officer (CMIO), the Center for Health Care Innovation (CHCI), and Clinical Effectiveness and Quality Improvement (CEQI) designed and implemented health informatics solutions in the form of Virtual Safety Nets (VSN)—innovative, patient-centered support systems.
The Information VSN started with a COVID-19 Hotline that directed over 18,000 callers to command centers, telemedicine resources, and a nurse triage team that had access to a constantly updated digital FAQ to provide the most accurate information on the virus.
The nurse triage team answered 8,500 calls, reassuring worried callers, assessing sick patients using a clinical protocol to assess severity of illness, and fielding questions about test results, testing sites, and when people could return to work.
For the Testing VSN, staff set up testing tents and ran COVID-19 tests not only for Penn Medicine patients, but others in the community, as well.
After patients were tested, the COVID-19 Results Management Center—comprised of 80 furloughed dermatology providers—followed up on more than 25,000 test results with a 33% positivity rate for COVID-19. These providers followed up with a phone call or with a telemedicine visit, providing answers about COVID-19 and directing patients to other services as needed.
The third VSN, for monitoring patients after they were tested for COVID-19, used an automated SMS-based program called COVID-Watch to text patients twice a day and ask about their symptoms, especially difficulty breathing.
When patients responded that their breathing was worse, they were immediately referred to a nurse and then to either the Emergency Department, Penn Medicine OnDemand telemedicine service, or their primary care provider, depending on the care they needed.
COVID-Watch followed patients for 14 days, with the possibility of extending monitoring for another 7 days if patients still had symptoms. When a provider called one 23-year-old patient enrolled in COVID-Watch who had tested positive for the virus, she could barely finish a sentence, had chest pain, and felt dizzy. She was reluctant to call an ambulance because she was worried that her neighbors would find out she had COVID-19. The provider called an ambulance for her, instructed the paramedics to turn off lights and sirens and to wear full PPE, and ensured that the patient would receive life-saving care.
Another tool in the Monitoring VSN was COVERS, a system that used automated texts or calls to screen patients for COVID-19 before in-person visits. This system saved hours of provider time and helped protect health care workers from being inadvertently exposed to COVID-19 during contact with patients.
The three VSNs, rolled out in a matter of weeks, impacted thousands of patients and ensured that no patient would be left behind.
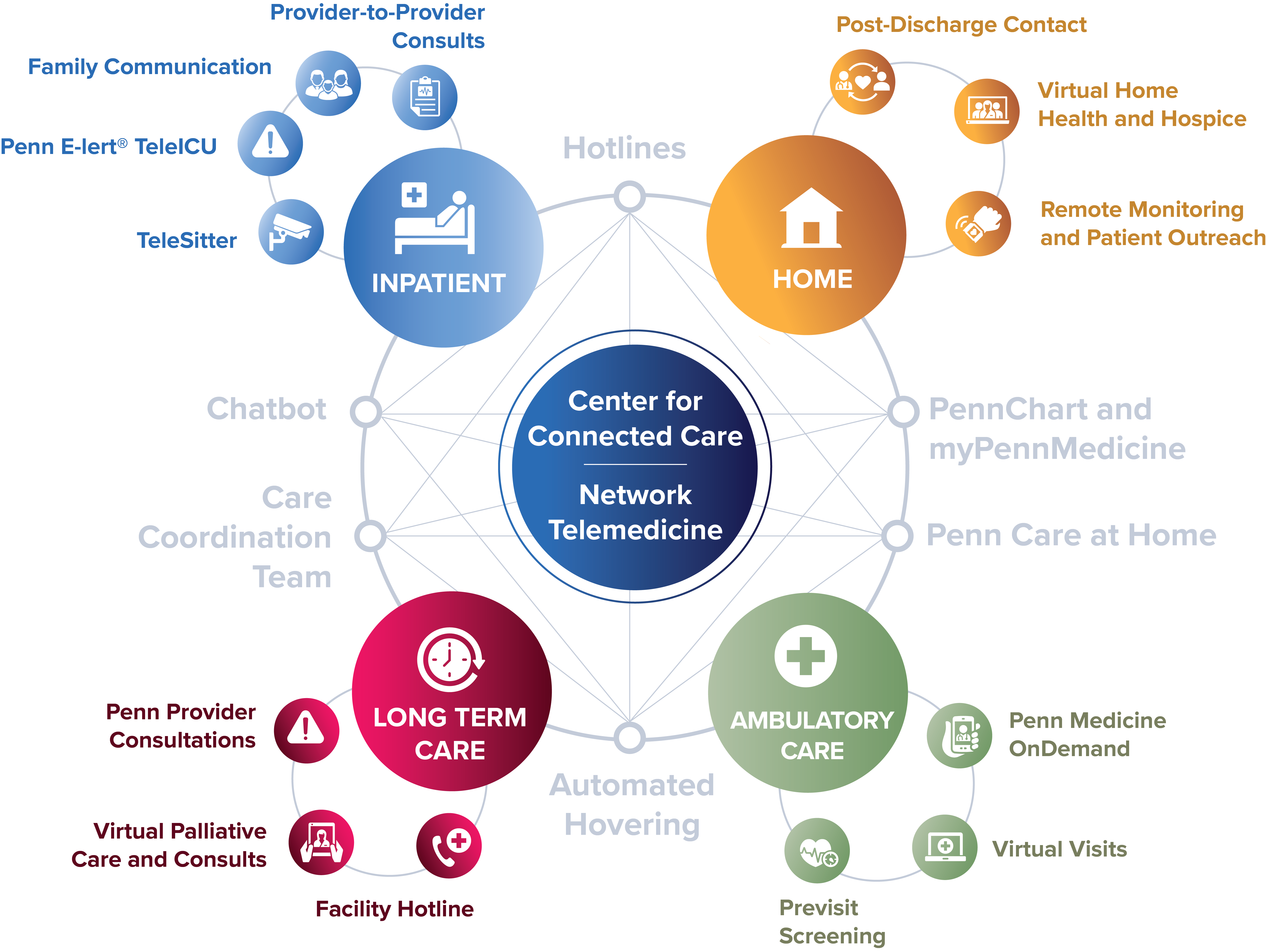
Before the pandemic, Penn Medicine handled about 1,000 telemedicine appointments per month. At peak volume, that number increased to 7,000 appointments per day.
The multidisciplinary team involved in this project registered more than 10,000 clinicians to take on telemedicine appointments and conducted almost 500,000 telemedicine appointments with patients.
Between March and June of 2020, the COVID-19 Hotline received about 18,000 calls—average call volume per day was 121 calls, with a peak weekday volume of 258 calls in early April. The Results Management Team made over 25,000 calls to ambulatory and Emergency Room patients with a 33% positivity rate for COVID-19.
As of June 2021, approximately 800 patients were enrolled in COVID-Watch. Of those patients, approximately 10-15% were referred to a telemedicine visit, to the Emergency Department, or directed to call 911.
Penn Medicine teams designed and implemented Virtual Safety Nets in order to provide a patient-centered support system for patients and the surrounding community. The multidisciplinary group of people working on the VSNs brought their own areas of expertise to bear in the project, and also relied on the strong informatics infrastructure already in place in the University of Pennsylvania Health System.